Take Control of Your Spine Surgery Journey
Preparing for spine surgery can feel overwhelming, but the right information empowers you to move forward with confidence. Understanding your diagnosis, exploring all your options, and knowing what to expect from surgery and recovery puts you in the driver’s seat of your own healthcare.
Dr. Joel Beckett is a leading spine surgeon who believes patients deserve more than a quick consultation and a surgical date. His approach centers on education and transparency; he wants you to fully understand your condition, weigh all treatment options, and make informed decisions that align with your health goals and lifestyle .
The questions you ask your surgeon matter as much as the answers you receive. Here are 15 essential questions to ask during your consultation, so you can evaluate your options clearly and make the best decision for your health and peace of mind.
1. What’s really causing my pain or symptoms?
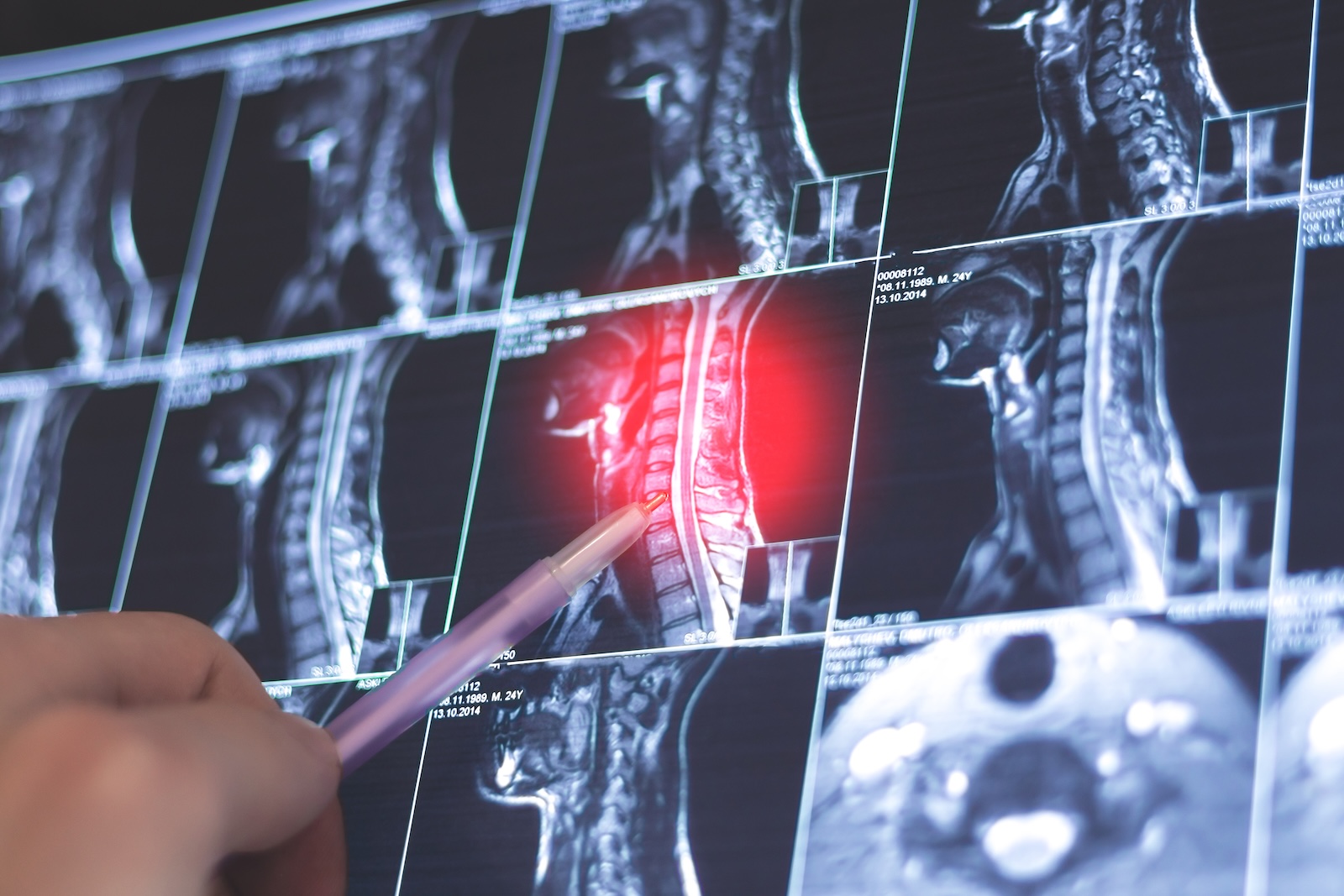
Ask your surgeon how they confirmed your diagnosis. Did they use MRI, CT scans, X-rays, or a combination? MRI shows soft tissues like discs and nerves, while CT scans show bone detail. But imaging alone isn’t enough. Dr. Beckett knows that accurate diagnosis requires correlating these images with your physical exam and symptoms.
Listen for a clear explanation that connects what the surgeon sees on your scans to your actual pain. Some people have abnormalities on imaging that don’t cause their symptoms, which is why this correlation matters.
Understanding the root cause helps you evaluate whether surgery truly addresses your problem and lets you explore all treatment options before committing to an operation.
2. Are there non-surgical options that could help first?
Unless it’s a medical emergency, surgery should never be your first option. Asking this question reveals whether your surgeon is committed to conservative care or simply eager to operate.
Non-surgical treatments include physical therapy, medications (anti-inflammatories or muscle relaxants), epidural steroid injections, nerve blocks, and newer approaches like acupuncture or regenerative medicine. Many spine conditions respond well to these conservative treatments, and research shows that aggressive conservative care can help patients avoid surgery altogether.
Dr. Beckett believes that truly skilled surgeons explore all non-surgical options before recommending an operation. Listen for a thorough explanation of what conservative treatments you should try first, how long to give them, and what outcomes to expect. If your surgeon rushes you toward surgery without discussing these alternatives, that’s a red flag.
3. What type of spine surgery do you recommend, and why?
This question helps you understand whether your surgeon has carefully considered which approach is best for your condition.
There are many different types of spine surgery, each designed for specific problems. Common procedures include discectomy (removing part of a herniated disc), laminectomy (removing bone to relieve pressure on nerves), spinal fusion (permanently connecting vertebrae), and disc replacement (replacing a damaged disc with an artificial one). Newer minimally invasive techniques can accomplish these same goals with smaller incisions, less tissue damage, and faster recovery times.
Dr. Beckett wants you to understand not just what procedure is recommended, but why it’s the right choice for your condition. Ask your surgeon to explain how the procedure will address your specific problem and why this approach is better than alternatives. For example, if fusion is recommended, why not disc replacement? If open surgery is suggested, is minimally invasive surgery an option? A surgeon who can clearly explain the reasoning behind their recommendation and acknowledge trade-offs between different approaches demonstrates expertise and transparency.
4. How experienced are you with this exact procedure?
Experience matters in spine surgery. Research shows that surgeons who perform higher volumes of spine procedures have lower complication rates, shorter hospital stays, fewer readmissions, and better outcomes than low-volume surgeons.
This question isn’t meant to be confrontational—it’s about gathering critical information. Ask your surgeon how many times they’ve performed your specific procedure, not just spine surgery in general. A surgeon who performs 100 disc replacements per year has vastly different experience than one who does five. Studies demonstrate that the relationship between surgeon volume and complications follows a dose-response pattern, meaning outcomes continue to improve as surgeons gain more experience.
Dr. Beckett encourages patients to ask directly about both the surgeon’s training (specialty certification and fellowship training) and their annual surgical volume for your specific condition. Listen for specific numbers, not vague reassurances (a range is okay). A confident, experienced surgeon will answer this question directly. If a surgeon seems defensive or unwilling to discuss their experience level, consider seeking a second opinion.
5. What are the potential risks or complications?
Every surgery carries risks, and spine surgery is no exception. A surgeon who openly discusses potential complications demonstrates honesty and helps you make an informed decision. This conversation shouldn’t scare you; it should prepare you and help you weigh whether the potential benefits outweigh the risks.
Common spine surgery complications include infection, bleeding, blood clots (deep vein thrombosis or pulmonary embolism), nerve damage, spinal fluid leaks (dural tears), and continuing or recurrent pain. More serious but less common risks include paralysis, stroke, or injury to blood vessels. Studies show that complication rates vary by procedure type, with more complex surgeries like spinal fusion and deformity correction having higher risk profiles. Certain patient factors such as age, obesity, diabetes, smoking, and previous spine surgery can increase your individual risk.
Dr. Beckett believes patients deserve realistic information about both short-term and long-term risks. A good surgeon will discuss your personal risk factors and explain what steps they take to minimize complications, such as proper surgical technique, infection prevention protocols, and blood clot prophylaxis.
6. What’s the success rate for patients like me?
General success rate statistics can be misleading because your outcome depends on your specific condition, health profile, and circumstances. This question pushes your surgeon to discuss your individual prognosis rather than offering broad reassurances.
Spine surgery success rates vary widely—from 60% to 95%—depending on the procedure type, diagnosis, and how “success” is defined. For example, discectomy (removing herniated disc material) shows 80-90% success in relieving leg pain, while more complex procedures may have different outcomes. Studies show that patients with clear, objective findings on imaging like a herniated disc visibly pressing on a nerve tend to have better results than those with vague pain that can’t be traced to a specific structural problem. Your personal factors matter too: age, overall health, smoking status, obesity, psychological factors, and previous spine surgeries all influence your chances of success.
Dr. Beckett wants you to have realistic expectations for your situation. Studies show that patient satisfaction is highest when expectations are clearly managed before surgery. A surgeon who can discuss both the percentage of patients who improve and what that improvement typically looks like gives you the information needed to make an informed decision.
7. What outcomes should I realistically expect?
Having realistic expectations before surgery is one of the strongest predictors of satisfaction afterward. This question forces an honest conversation about what surgery can and cannot accomplish for your specific condition.
Surgery typically improves symptoms but rarely eliminates them completely. Research demonstrates that 81% of patients report their expectations were met after spine surgery, but this only happens when those expectations were realistic from the start. Patients with unrealistic or overly high expectations often experience disappointment even when the surgery achieves good clinical results.
Dr. Beckett emphasizes discussing specific, measurable outcomes rather than vague promises. Patients who perceive their general health as good before surgery tend to have better outcomes than those who view their overall health as poor, so your surgeon should consider your whole health picture when predicting your outcome.
8. What kind of imaging or diagnostics do you rely on before surgery?
The quality of your surgery depends heavily on the quality of the diagnostics that guide it. Comprehensive preoperative imaging typically includes MRI (the gold standard for visualizing soft tissues like discs, nerves, and ligaments), CT scans (for detailed bone anatomy and surgical planning, especially for screw placement), and/or X-rays with flexion and extension views (to assess spinal stability). Not all of these are always necessary, but they may be in complex cases. Also in complex cases, surgeons may use specialized imaging like SPECT scans to identify the exact source of pain, or angiography to map blood vessel anatomy before surgery on the upper spine.
Dr. Beckett emphasizes that multiple imaging studies can provide different critical information that guides surgical decisions. Ask your surgeon which imaging they’re using and why each test matters for your procedure. A thorough surgeon will correlate findings across different imaging types to confirm their diagnosis and plan the safest approach.
9. How long will recovery take, and what does it look like?
Understanding your recovery timeline is essential for planning time off work, arranging help at home, and setting realistic expectations. Recovery varies dramatically depending on the type of surgery. Asking this question helps you prepare practically and mentally for what’s ahead.
Recovery timelines differ significantly by procedure type. Minimally invasive surgeries like discectomy typically allow return to light activity in 2-4 weeks and normal activity around 6 weeks. Moderate procedures like laminectomy or artificial disc replacement usually require 4-6 weeks for light activity and 8-12 weeks for normal activity. More extensive surgeries like spinal fusion take much longer—6-8 weeks before resuming light activity and 3-6 months or more for full recovery as the bone fusion heals.
Dr. Beckett wants you to ask specific questions about your recovery timeline. When can you drive, return to work, lift objects, exercise, or resume sports? What will physical therapy involve and for how long? Studies show that return to sports and high-impact activities typically occurs 4-6 months after surgery, pending surgeon approval. A surgeon who provides detailed, milestone-based recovery information helps you plan your life and understand what “normal” looks like at each stage.
10. Will I need physical therapy or rehabilitation?
Physical therapy is almost always a part of spine surgery recovery, yet many patients don’t realize this until after their procedure. Asking this question upfront helps you plan for the time commitment and understand that surgery is only the first step in your recovery journey.
Surgery addresses the structural problem, but physical therapy helps your body learn to function optimally with these changes. Research shows that patients who engage in post-surgical physical therapy experience significantly reduced pain, improved spinal function, better mobility, and faster return to daily activities.
Dr. Beckett wants you to understand what your rehabilitation will involve. A typical program progresses through phases: early focus on pain management and basic movement, then strengthening your core and back muscles, and finally restoring full function and returning to activities. Ask your surgeon how long physical therapy will last, how many sessions per week you’ll need, and what specific goals you’re working toward. Without proper rehabilitation, you risk delayed healing, muscle weakness, reduced flexibility, and chronic pain.
11. What are my options for pain management after surgery?
Pain management is a critical part of your recovery. Asking this question upfront helps you understand your options and avoid over-reliance on opioid medications, which carry risks of dependence and side effects.
Your pain management plan may include non-opioid medications like NSAIDs (nonsteroidal anti-inflammatory drugs such as ibuprofen), acetaminophen, and gabapentinoids (medications that treat nerve pain), all of which have been shown to reduce opioid use and improve pain scores after spine surgery. Regional techniques such as nerve blocks, epidural analgesia, or local anesthetic wound infiltration can provide targeted pain relief at the surgical site. Research also shows that alternative approaches like acupuncture, transcutaneous electrical nerve stimulation (TENS), cold therapy, and cognitive behavioral therapy can complement medication-based strategies.
Dr. Beckett believes patients should know their full range of options before surgery. Ask your surgeon what combination of medications and techniques they’ll use, how long you’ll need pain medication, and what non-medication strategies can help. Understanding that opioids may be necessary short-term but should be minimized helps you set realistic expectations.
12. Will surgery limit my mobility or flexibility long-term?
The answer depends entirely on which type of surgery you’re having, and understanding this trade-off is essential before you commit. Spinal fusion permanently eliminates movement at the fused segment, reducing your ability to bend, twist, or flex at that location. Motion-preserving surgeries like artificial disc replacement maintain spinal flexibility while still relieving pain, offering an alternative that doesn’t sacrifice mobility.
Dr. Beckett wants you to ask specifically how many levels are being fused and what percentage of motion you’ll lose. A surgeon who discusses both the mobility limitations and the potential for adjacent segment degeneration (new problems developing at neighboring spine levels) demonstrates honesty and helps you make an informed decision.
13. If an implant is used, how long does it last?
Many spine surgeries use hardware like rods, screws, cages, or artificial discs, and understanding their lifespan helps you plan for the future. This question reveals whether you might need additional surgery down the road and what long-term maintenance your spine will require.
Artificial disc replacements typically last 10-20 years or longer, with some studies suggesting they could last 40-70 years or even a lifetime for most patients. Spinal fusion hardware (cages, rods, and screws) is designed to last permanently once the bones fuse together, though the hardware itself can occasionally break down over time, requiring revision surgery.
Dr. Beckett wants you to ask what type of implant will be used and what the long-term failure or revision rates are for that specific device. A surgeon who discusses realistic expectations about implant longevity and the possibility of future surgery demonstrates transparency and helps you make a fully informed decision.
14. What kind of follow-up care do you provide?
Your relationship with your surgeon shouldn’t end when you leave the operating room, and ongoing monitoring is essential for catching complications early and ensuring optimal healing.
Comprehensive follow-up typically includes scheduled appointments at 1-3 weeks (for wound evaluation), 3 months (for bony healing assessment), 6 months, and 1 year post-surgery, with imaging studies at key milestones to monitor healing and hardware integrity. Surgeons should also assess your pain levels, functional improvement, neurological status, and rehabilitation progress throughout your recovery.
Dr. Beckett emphasizes that patients deserve clear information about how accessible he’ll be after surgery and what long-term monitoring looks like. Ask how many follow-up appointments you’ll have, what each appointment will assess, and how to reach your surgeon if complications arise between visits.
15. How can I prepare now for the best possible outcome?
What you do before surgery can make a huge difference in how well you heal and how quickly you recover. The steps you take in the weeks leading up to your procedure give you real control over your results.
The most important preparations include quitting smoking (at least 4-6 weeks before surgery), reaching a healthy weight if possible, keeping your blood sugar and blood pressure under control, eating protein-rich foods, and doing gentle exercises to strengthen your core. Research shows that patients who take these steps before spine surgery have fewer complications, shorter hospital stays, and better satisfaction with their results.
Dr. Beckett wants you to ask what specific actions you should take to get your body ready for surgery. A surgeon who gives you a personalized preparation plan shows they’re invested in your success, not just the operation itself.
Red Flags to Watch For
Not all spine surgeons approach patient care the same way, and certain warning signs should make you think twice about moving forward. Recognizing these red flags can help you avoid surgeons who prioritize procedures over your well-being.
Be cautious if a surgeon rushes you into surgery without ordering comprehensive diagnostic imaging or exploring conservative treatments first. Another warning sign is a surgeon who can’t or won’t clearly explain your diagnosis, surgical alternatives, potential risks, or realistic outcomes in terms you understand. If your consultation feels rushed, dismissive, or one-sided—with little opportunity for you to ask questions—that’s a problem.
Finally, pay attention if there’s minimal discussion about recovery timelines, physical therapy requirements, or long-term effects on your mobility and lifestyle. A surgeon who focuses only on the procedure itself without addressing what comes after may not have your long-term interests at heart. Trust your instincts—if something feels off or you’re being pressured, seeking a second opinion is always appropriate and often reveals important information.
An Informed Patient Heals Better
Walking into your consultation with a written list of questions empowers you to take control of your spine health journey. Dr. Beckett’s approach centers on education, transparency, and personalized care. He believes you deserve to fully understand your diagnosis, explore all your options, and know exactly what to expect from surgery and recovery. When you’re informed and involved in your care, you’re more likely to follow your treatment plan, experience better outcomes, and feel satisfied with your results.
If you’re exploring spine surgery, schedule a consultation with Dr. Beckett to discuss your options and get a clear roadmap for recovery. Bring this list of questions with you, and don’t hesitate to ask for clarification on anything that’s unclear. Your spine health is too important to leave to chance.